Sort 1 diabetes is brought on by an autoimmune assault that destroys the beta cells, the a part of the physique that produces the important hormone insulin. It’s usually supposed that when these cells have been misplaced, they’re gone endlessly. Within the seek for a remedy, essentially the most superior analysis has focused on the transplantation of recent beta cells — both from an organ donor or grown in a laboratory — to exchange the cells which were irrevocably misplaced.
However what in case your physique could possibly be directed to regrow its personal new beta cells? A lead investigator on the Diabetes Analysis Institute believes that the pancreas can regenerate beta cells, and that his lab has found make it occur.
A Century of Questions
Many human cells can regenerate themselves. You could have heard that, attributable to fixed cell regrowth, your entire human physique is changed each seven years. That’s not fairly proper — whereas most of your pores and skin cells flip over inside months, you even have mind cells that by no means have been and by no means might be changed.
The pancreas, like most different inner organs, is sluggish to regenerate and has a really restricted capacity to heal itself. However medical doctors have lengthy suspected that the pancreas harbors the power to regenerate the islet cells, which comprise the insulin-producing beta cells. “The idea has been round for greater than 100 years,” since even earlier than the invention of insulin, says Juan Dominguez-Bendala, PhD. It’s all the time been a controversial thought, however he believes that the talk has now been settled.
Dr. Dominguez-Bendala is the Director of Stem Cell & Pancreatic Regeneration and Analysis on the Diabetes Analysis Institute. His crew, in a collaborative effort along with his colleague Dr. Ricardo Pastori, just lately revealed a report in Cell Metabolism that lastly proves that the grownup human physique is able to rising new beta cells:
“I feel that that is very definitive. We’re regeneration in the actual factor, the actual human pancreas. We see this occurring in real-time. It’s unequivocal.”
New Proof
The islet cells that comprise each the beta cells and different necessary exocrine cells solely make up a small minority of the pancreas’ mass. Many of the organ is dedicated to a ductal system that helps synthesize digestive juices and transport them to the intestines. Within the embryo, although, this a part of the pancreas additionally creates the islet cells.
“There are many people who don’t consider that it is a course of that occurs throughout regular grownup life. However what we and others contend is that when there’s intensive harm to the pancreas, there’s a partial reactivation of the embryonic program that led to islet cells within the first place. There are stem cells within the ducts that give rise to new islets.”
For years, nevertheless, the proof in favor of human islet regeneration solely got here within the type of samples from the pancreases of deceased individuals. It had by no means been doable to watch the regeneration of islet cells in real-time, and “the proof was quite circumstantial.” There was supporting proof from mouse fashions, however Dominguez-Bendala admits that this was of restricted worth: “We now have cured diabetes in mice a whole lot of various methods, and none of them have ever labored in people.”
Scientists acquired a brand new software with the institution of nPOD, the Community for Pancreatic Organ Donors with Diabetes. Based and supported by the main charity JDRF, nPOD encourages individuals with diabetes to enroll as organ donors and donate their pancreases to science. This nationwide community is the one manner for American researchers to obtain a dependable provide of viable organs from individuals with kind 1 diabetes.
Dominguez-Bendala’s lab started receiving donations of pancreas slices in 2018. It took some tinkering, however they discovered a medium that “might lengthen the life and performance in vitro for about two weeks, which was loads for us to begin seeing if there’s regeneration.” It supplied, for the primary time, “a window into the actual pancreas.”
The best way to Stimulate Beta Cell Regeneration
If pancreatic regeneration does happen naturally, it’s clearly not sufficient to considerably heal individuals with diabetes or pancreatitis. To make a distinction, Dominguez-Bendala must discover a technique to speed up and amplify the regeneration course of. His secret ingredient could also be a pure human development issue named BMP7.
BMP7 is “like a gas for stem cells throughout the physique,” and Dominguez-Bendala needed to see if it might have the identical impact within the pancreas. The substance is well-studied and is already accepted for an unrelated situation: “It’s already in medical use. It regrows bone, and is used to fuse vertebrae when you’ve spinal surgical procedure.”
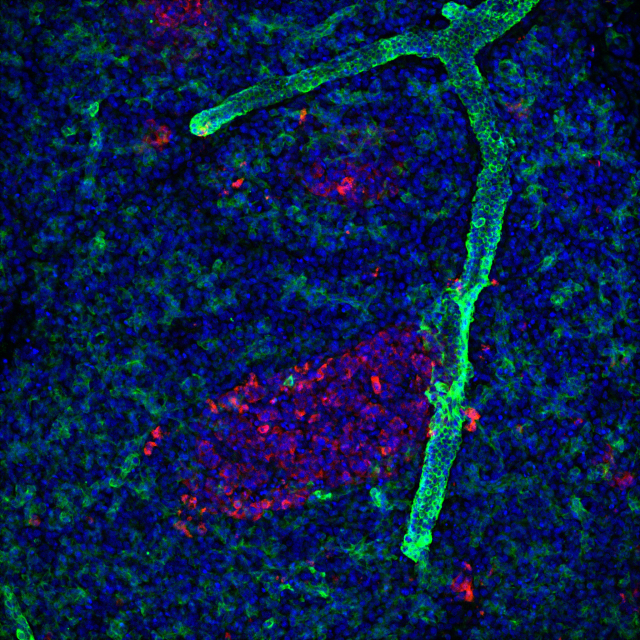
The crew at Dominguez-Bendala’s lab would take a number of pancreatic slices from a single donor and handled some with BMP7. Once they took a more in-depth look, they noticed precisely what they’d hoped: new hybrid cells rising from the ductal mass of the pancreas and making a bridge in direction of the realm the place islet cells are born. A trajectory evaluation confirmed that among the new hybrid cells “grew to become new islet cells.”
“We confirmed for the primary time, in a human-based mannequin, how regeneration works.”
“We found that progenitor cells contained in the ducts reply to BMP7 by proliferating, after which while you take away the BMP7, they differentiate into all of the completely different cell varieties of the pancreas.”
“To me, it doesn’t get any extra promising than that,” Dominguez-Bendala stated. “You’ll be able to remedy diabetes left and proper in mice, however to indicate that you could induce beta cell regeneration in a sort 1 diabetes donor? That’s one thing actually main.”
Subsequent, they needed to show that the brand new islet cells had been truly useful. May they reply to excessive blood sugar ranges, secrete insulin, and proper hyperglycemia? “Once we take a look at the neogenic cells, the cells which were fashioned because of BMP7 stimulation, we are able to see that they reply to glucose stimulation by making insulin.”
It’ll take a number of years and “lots of boring experiments” to persuade the FDA that the remedy is secure to strive in people. Research of mice, at the very least, present that BMP7 causes no different dysfunctional tissue development. It additionally doesn’t stimulate islet cell development in wholesome mice, suggesting that the substance naturally targets accidents: “We predict it takes an excessive diploma of injury to the pancreas for this very primitive regeneration program to be activated.” Research in people assist present that BMP7 is secure for common use, together with when used to assist heal kidney illness.
The Immunity Drawback
Beta cell regeneration has the identical large drawback that each different proposed kind 1 diabetes remedy has: the immune system. Transplanted islet cells — whether or not they come from an organ donor or a laboratory manufacturing course of — can appropriate hyperglycemia and grant insulin independence, however to this point no one has found out shield them from the immune system with out the usage of highly effective medication (with doubtlessly highly effective unwanted side effects).
“This doesn’t work except we do one thing concerning the immune system, or else the brand new cells might be destroyed time and again,” says Dominguez-Bendala. “We envision this as a mix remedy alongside immunotherapies.”
Dominguez-Bendala is playing, together with the remainder of the diabetes world, that higher immunotherapies are coming quickly. In the mean time, the primary affected person inhabitants prone to profit from any beta cell regeneration remedy are individuals who have acquired a kidney transplant, sufferers who due to this fact already require anti-rejection medicines.
There’s at the very least some hope, nevertheless, that naturally regenerated beta cells might be simpler to guard from the immune system than transplanted cells, which the physique’s defenses establish as international. We gained’t know but how the physique will reply to neogenic cells: “The reality is that we don’t know. I’ve spoken to immunologists who consider that the brand new cells could possibly sneak in and gained’t be destroyed as rapidly as those that had been destroyed within the first place. I’m hopeful that it’s going to occur, however I’m not relying on that.”
Timeline
Beta cell regeneration is in its infancy as a remedy, and would require a few years of experimentation earlier than it will get wherever near FDA approval. I requested Dominguez-Bendala if a extra superior potential remedy — akin to Vertex’s VX-264 — may succeed first and render his work out of date. Dominguez-Bendala doesn’t see Vertex as a competitor — his lab has helped contribute to progress within the area of stem cell differentiation — however he’s emphatic that VX-264 is not going to be a full remedy and won’t finish the seek for higher kind 1 diabetes treatments:
“It’s not a remedy by any stretch of the creativeness. It’s a brute power technique, placing issues within the physique, and the physique is attacking them. What we’re proposing is basically completely different, to harness the very pure capacity of the pancreas to heal itself. That’s a way more holistic strategy.”
A number of different analysis teams are investigating parallel therapies. In France, a startup named DiogenX believes it has discovered one other technique to regenerate the beta cells. And simply final week, an Australian crew revealed a research of one other methodology that would stimulate beta cell regeneration.
“I’m hopeful that it is going to be obtainable sooner quite than later. We might spend twenty years exploring the little particulars of the mechanisms, however that’s not what the Diabetes Analysis Institute is about. We need to have therapies within the clinic as quickly as doable. That’s our mission, and that’s what we’re going to do.”